What is Substance Use Treatment?

Understanding Substance Use Treatment
Substance use treatment plays a crucial role in addressing substance use disorders (SUDs) and supporting individuals on their journey to recovery. It encompasses various therapies, medications, support groups, and treatment programs tailored to meet the specific needs of individuals struggling with addiction.
Overview of Substance Use Disorders
Substance use disorders refer to a range of conditions characterized by the recurrent use of substances despite the negative consequences they may cause. These substances can include alcohol, opioids, stimulants, sedatives, and more. Substance use disorders are chronic diseases that affect the brain and behavior, and they require comprehensive treatment to manage effectively.
In 2017, it was estimated that 20.7 million Americans needed treatment for substance use disorders, but only 2.5 million received specialized substance use treatment [2]. This treatment gap highlights the importance of increasing access to evidence-based interventions for those struggling with addiction.
Statistics on Treatment Disparities
Despite the significant need for substance use treatment, disparities exist in the utilization of these services. Factors such as socioeconomic status, race, ethnicity, and geographic location can influence access to and utilization of treatment services.
It is crucial to address these disparities and ensure that everyone has equal opportunities to receive effective treatment. By providing accessible and culturally appropriate treatment options, individuals from all backgrounds can access the help they need.
Statistics indicate that in 2020, an estimated 6.7% of adults aged 18 or older (approximately 17 million people) had a co-occurring mental illness and substance use disorder (SUD) [3]. This highlights the importance of integrated treatment approaches that address both mental health and substance use disorders. By treating these conditions concurrently, individuals have a better chance of achieving successful outcomes and maintaining long-term recovery.
Understanding substance use treatment and the disparities that exist in accessing these services is crucial for developing effective strategies to improve treatment outcomes and support individuals on their path to recovery. By addressing the unique needs of individuals with substance use disorders, we can work towards reducing the impact of addiction and promoting healthier, fulfilling lives.
Types of Behavioral Therapies
Behavioral therapy is a widely used and effective approach in the treatment of substance use disorders. It encompasses several techniques that aim to modify harmful behaviors and promote positive change. In this section, we will explore the role of behavioral therapy, as well as two specific types: Cognitive Behavioral Therapy (CBT) and Contingency Management.
Role of Behavioral Therapy
Behavioral therapy plays a crucial role in substance use treatment. It helps individuals understand the underlying causes and triggers of their addictive behaviors, as well as develop healthier coping mechanisms. By addressing the thoughts, feelings, and behaviors associated with substance use, behavioral therapy can empower individuals to make positive changes and lead a life free from addiction.
Behavioral therapy has been adapted into various techniques that cater to the unique needs of individuals seeking treatment for substance use disorders [2]. These techniques are typically delivered by trained therapists or counselors who specialize in addiction treatment.
Cognitive Behavioral Therapy (CBT)
Cognitive Behavioral Therapy (CBT) is a widely recognized and evidence-based form of therapy that has shown positive and lasting impacts on individuals struggling with substance misuse. CBT focuses on identifying and modifying dysfunctional thoughts, emotions, and behaviors that contribute to addiction.
During CBT sessions, individuals learn to challenge and reframe negative thought patterns that may drive their addictive behaviors. They also acquire practical skills and strategies to manage cravings, cope with stress, and handle situations that may trigger substance use.
The skills learned in CBT tend to "stick" with individuals beyond the completion of treatment, making it a valuable tool in maintaining long-term recovery. CBT can be provided in individual or group therapy settings, depending on the individual's needs and preferences.
Contingency Management
Contingency Management is a behavioral therapy approach that utilizes positive reinforcement to promote abstinence and encourage positive behaviors. This technique has shown effectiveness in treating various substance use disorders, including those involving alcohol, stimulants, opioids, and marijuana.
In a Contingency Management program, individuals receive tangible rewards, such as vouchers or cash prizes, for achieving specific treatment goals, such as abstinence from substances or attending counseling sessions. By providing immediate and tangible incentives, Contingency Management helps reinforce positive behaviors and motivate individuals to maintain their recovery efforts.
The rewards offered in Contingency Management programs are carefully designed to promote sobriety and healthy behaviors. As treatment progresses, the frequency and value of the rewards may be adjusted to encourage continued progress and sustained recovery.
By utilizing behavioral therapy techniques such as CBT and Contingency Management, individuals undergoing substance use treatment can gain the necessary tools and skills to overcome addiction. These therapies, when combined with other treatment modalities, provide a comprehensive approach that addresses the complexities of substance use disorders and supports individuals on their journey to recovery.
Medications in Addiction Treatment
Medications play a crucial role in many substance use treatment plans, working in conjunction with counseling and behavioral therapies to enhance recovery outcomes. They are used to reduce cravings, manage withdrawal symptoms, and support individuals throughout their journey to recovery. In this section, we will explore the importance of medications in addiction treatment, as well as specific medications used for opioid withdrawal and alcohol and sedative withdrawal.
Importance of Medications
Medications are an integral part of many effective addiction treatment protocols. When combined with counseling and behavioral therapies, medications can help individuals navigate the challenges of withdrawal, reduce cravings, and minimize the risk of relapse [2]. They are prescribed based on an individual's specific needs and the type of substance use disorder they are facing.
Medications for Opioid Withdrawal
Opioid withdrawal can be a challenging and uncomfortable process. Medications are commonly used to manage withdrawal symptoms and reduce cravings. Some of the medications used during opioid withdrawal include:
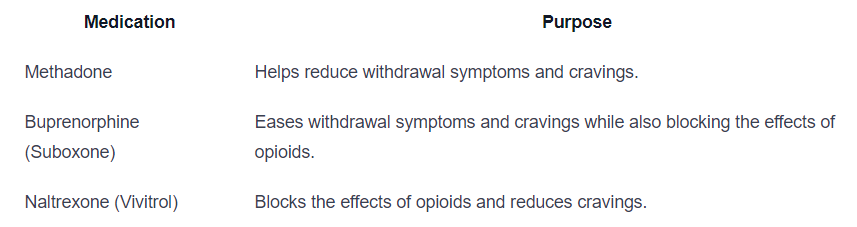
These medications are typically used during detoxification to alleviate symptoms such as anxiety, muscle aches, and cravings [4]. Dosages may be adjusted throughout the recovery journey to ensure the best chance of achieving and maintaining sobriety.
Medications for Alcohol and Sedative Withdrawal
Withdrawal from alcohol and sedatives can be severe and potentially life-threatening. Medications are commonly used to manage withdrawal symptoms, reduce cravings, and support individuals during the recovery process. Some of the medications used for alcohol and sedative withdrawal include:
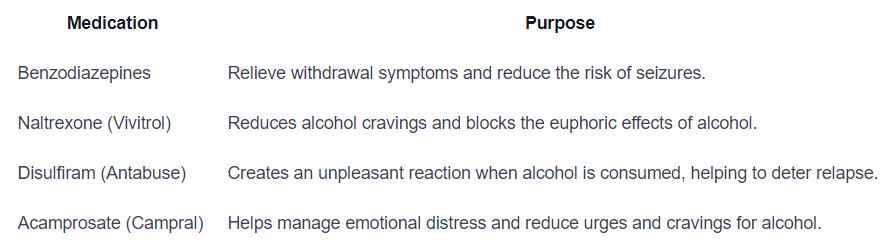
These medications are utilized during detoxification and beyond, supporting individuals through post-acute withdrawal syndrome (PAWS) [4]. PAWS can persist for up to two years after initial detox, and medication management during this phase helps individuals cope with emotional distress and reduce the likelihood of relapse.
It's important to note that medication management is often integrated into comprehensive treatment programs, whether in an inpatient (residential) or outpatient setting. Dosages and medication regimens are adjusted based on individual needs and progress, ensuring the best possible outcomes for long-term recovery.
Co-occurring Mental Health Disorders
Individuals struggling with substance use disorders often face co-occurring mental health disorders, necessitating a comprehensive treatment approach. It is estimated that about 6.7% of adults aged 18 or older, approximately 17 million people, have a co-occurring mental illness and substance use disorder (SUD) Recovery.org. The strong links between substance use and mental health underscore the importance of seeking treatment that addresses both aspects of an individual's well-being.
Dual Diagnosis: Mental Health & Substance Use
A dual diagnosis refers to the presence of both a mental health disorder and a substance use disorder. The co-occurrence of these conditions can complicate treatment and recovery, as they often influence and exacerbate each other. For example, individuals with mental health conditions may be more likely to misuse substances like alcohol.
To effectively address co-occurring disorders, treatment approaches must take into account the unique needs of individuals. Treatment plans should be designed to address physical, psychological, emotional, and social issues, in addition to substance use. This comprehensive approach aims to provide holistic care, ensuring that individuals receive the support they need to address both their mental health and substance use challenges Partnership to End Addiction.
Treatment Approaches for Co-occurring Disorders
Treating co-occurring disorders requires an integrated approach that combines mental health services and substance use treatment. This approach acknowledges that both conditions are interconnected and should be addressed simultaneously.
Effective treatment for co-occurring disorders typically involves a combination of therapies, such as:
- Medication-Assisted Treatment (MAT): Medications are often used to manage withdrawal symptoms and cravings associated with substance use disorders. Medications may be prescribed as part of an inpatient or outpatient treatment program, with dosages adjusted during treatment to optimize recovery Addiction Center.
- Behavioral Therapy: Various forms of behavioral therapy, such as cognitive-behavioral therapy (CBT) and contingency management, can help individuals address both their mental health and substance use challenges. These therapies aim to identify and modify harmful thoughts, beliefs, and behaviors, promoting healthier coping mechanisms and reducing substance misuse NIDA.
- Support Groups and Peer Support: Engaging in support groups, such as 12-step programs or other recovery support networks, can provide individuals with co-occurring disorders a sense of community and understanding. Peer support offers valuable insights and encouragement, promoting long-term recovery.
By addressing co-occurring mental health and substance use disorders concurrently, individuals can receive the comprehensive care they need to achieve and maintain recovery. Treatment programs that integrate various therapeutic approaches and support systems have been shown to be effective in helping individuals navigate the complexities of co-occurring disorders.
Support Groups in Recovery
Support groups play a significant role in the recovery process for individuals with substance use disorders. These groups provide a safe and supportive environment where individuals can share experiences, gain insights, receive emotional support, and build connections. The benefits of actively participating in support groups are numerous, contributing to overall well-being and success in overcoming substance use disorder.
Role of Support Groups
Support groups for substance use disorder recovery come in various forms, catering to individuals with different preferences and needs. Examples include 12-step programs, SMART Recovery, and peer-led groups [5]. The primary role of support groups is to provide individuals with a space where they can connect with others who have similar experiences and challenges. These groups offer understanding, empathy, and encouragement, fostering a sense of community and belonging.
In addition to emotional support, support groups provide individuals with access to valuable resources. Members can learn about different coping strategies, treatment options, and local resources that can aid in their recovery journey. Support groups also promote accountability and motivation, as members hold each other responsible for their actions and progress.
Different Types of Support Groups
Support groups in substance use disorder recovery differ in terms of structure, approach, and focus. Some widely known support groups include:
- 12-Step Programs: Examples include Alcoholics Anonymous (AA) and Narcotics Anonymous (NA). These programs follow a structured approach based on twelve steps that guide individuals towards sobriety and personal growth.
- SMART Recovery: This program focuses on self-empowerment and teaches practical tools and techniques for managing addictive behaviors. It incorporates elements of cognitive-behavioral therapy (CBT) and motivational interviewing.
- Peer-Led Groups: These groups are often facilitated by individuals who have personal experience with substance use disorder and are in recovery themselves. Peer-led groups provide a unique perspective and understanding, as facilitators can relate to the challenges faced by members.
The choice of the support group depends on individual preferences and needs. Therapists or treatment providers can assist individuals in finding the right support group that aligns with their goals and provides the necessary support.
Benefits of Active Participation
Active participation in support groups is crucial for maximizing the benefits of these groups. By actively engaging in group discussions, sharing experiences, and offering support to others, individuals can enhance their recovery journey. Some key benefits of active participation include:
- Resource Sharing: Members can exchange valuable information about treatment options, coping strategies, and local resources, providing each other with practical tools for managing substance use disorder.
- Coping Skills Development: Support groups offer a platform for learning and practicing coping skills. Members can share effective strategies they have discovered and receive feedback from others, enhancing their ability to navigate challenges and triggers.
- Sense of Community: Participating in support groups creates a sense of belonging and community. Knowing that others understand their struggles and successes can foster a supportive environment that encourages continued progress.
- Accountability and Motivation: Support groups promote accountability by holding members responsible for their actions and progress. This accountability, combined with the motivational atmosphere of the group, can be a powerful driving force for sustained recovery.
By actively participating in support groups, individuals can tap into these benefits and enhance their overall recovery experience. The shared journey, guidance, and support from fellow group members can make a significant difference in successfully overcoming substance use disorder.
Treatment Programs & Settings
When seeking substance use treatment, individuals have access to various programs and settings tailored to their specific needs. Understanding these treatment options is essential for making informed decisions regarding one's recovery. In this section, we will explore detoxification programs, the difference between inpatient and outpatient treatment, as well as intensive outpatient and partial hospitalization programs.
Detoxification Programs
Detoxification programs play a crucial role in the substance abuse treatment process. These programs involve the supervised process of clearing the body from substances and managing withdrawal symptoms. Medical supervision during detox is important to ensure individuals remain safe and effectively manage any uncomfortable or dangerous withdrawal symptoms they may experience.
The primary goal of detoxification is to reduce life-threatening medical events related to acute substance withdrawal. The duration of the detox process can vary, lasting from several days to weeks. It is vital to work with medical professionals during this phase to effectively manage withdrawal symptoms and ensure a safe transition into further treatment.
Inpatient vs. Outpatient Treatment
Inpatient and outpatient treatment are two primary options for substance use treatment.
Inpatient treatment, also known as residential or rehab programs, provides treatment in a residential setting. These programs typically last from one month to a year, and residents progress through different phases during the program. In certain phases, contact with family members may be limited. Inpatient programs offer a range of services, including therapy, counseling, education, vocational training, and more.
On the other hand, outpatient treatment programs involve attending treatment sessions at a specialty facility while living at home. These programs offer low to medium intensity, with clients attending no more than nine hours of treatment per week. Services in outpatient programs are often provided in the evenings and weekends to accommodate individuals who need to continue working or attending school [6].
Intensive Outpatient & Partial Hospitalization Programs
For individuals with specific needs or accompanying medical or psychological issues, intensive outpatient and partial hospitalization programs offer more concentrated treatment.
Intensive Outpatient Programs (IOP) provide medium to high intensity treatment, with clients attending 10-20 hours of treatment per week at a specialty facility while living at home. This option is suitable for individuals who require multiple services or have not succeeded in outpatient treatment. IOPs offer comprehensive therapy, counseling, and support services to aid individuals in their recovery journey [6].
Partial hospitalization programs (PHP) involve a higher level of care, with individuals attending treatment for up to five days a week, several hours each day. These programs are well-suited for individuals who require structured support but do not need 24-hour supervision. PHPs provide intensive therapy and support, allowing individuals to receive treatment while still residing at home or in a sober living environment [6].
By understanding the various treatment programs and settings available, individuals can choose the option that aligns best with their needs and goals for recovery. It's important to consult with healthcare professionals or addiction specialists to assess which program or setting is most suitable for each individual's unique circumstances.
References
[1]: https://nida.nih.gov/publications/drugs-brains-behavior-science-addiction/treatment-recovery
[2]: https://americanaddictioncenters.org/therapy-treatment
[3]: https://recovery.org/drug-treatment/types-of-programs/
[4]: https://www.addictioncenter.com/treatment/medications/
[5]: https://concertedcaregroup.com/the-role-of-support-groups-in-substance-use-disorder-recovery/
[6]: https://drugfree.org/article/types-of-addiction-treatment/
